Acinetobacter baumannii (A. baumannii ) poses a significant and growing threat within U.S. hospitals, impacting over one in one hundred patients. This bacterium is notorious for its adaptable genome and rapid development of antibiotic resistance, making infections difficult to treat and often leading to severe consequences.
The Rising Threat of A. baumannii Infections
The concern surrounding A. baumannii is underscored by research indicating that approximately one-third of hospital-acquired infections by this bacterium in the U.S. demonstrate resistance to carbapenems, a crucial class of antibiotics. These resistant infections are associated with increased mortality rates, prolonged hospital stays, and frequent transfers to other healthcare facilities – outcomes that highlight the urgency of understanding and combating this bacterial threat.
Mapping Resistance Mechanisms: An Experimental Evolution Approach
Researchers at Sanford Burnham Prebys and Roche Pharmaceuticals have recently published findings in Antimicrobial Agents and Chemotherapy, detailing a new approach to map the genetic mutations driving antibiotic resistance in A. baumannii. Their method utilizes an “experimental evolution” technique, focusing on two uncommon antibiotics, tigecycline and colistin – often considered last-line defenses against A. baumannii infections.
“These antibiotics represent physicians’ last resort for A. baumannii infections,” explained Andrei Osterman, Ph.D., a professor involved in the research. “While resistance is currently relatively low in the U.S., it is rising, prompting our investigation into how these bacteria acquire new resistance mechanisms.”
The Morbidostat: A Bacterial Evolution Machine
The team’s innovative approach leverages a specialized device called a morbidostat. This system enables continuous bacterial growth under escalating antibiotic pressure across multiple generations. A computer controls the process, monitoring the culture’s growth rate and progressively introducing increasing concentrations of the antibiotic drug, effectively mimicking conditions within the human body – a more realistic scenario than traditional laboratory methods.
“Think of it as an evolution machine,” Osterman described. “Combined with genomic sequencing, it allows us to construct a comprehensive map of virtually all possible mutations that confer antibiotic resistance.”
Key Findings: Resistance Pathways for Tigecycline and Colistin
The researchers’ mapping efforts successfully confirmed and broadened existing knowledge regarding the primary mechanisms of resistance to both tigecycline and colistin. For tigecycline, the most common route to resistance involves mutations that enhance the activity of efflux pumps – systems within the bacteria that isolate and remove the drug before it can damage the cell.
“This is a well-established mechanism,” Osterman noted, “and our findings significantly expand our understanding of the range of mutations involved in driving tigecycline resistance in A. baumannii.”
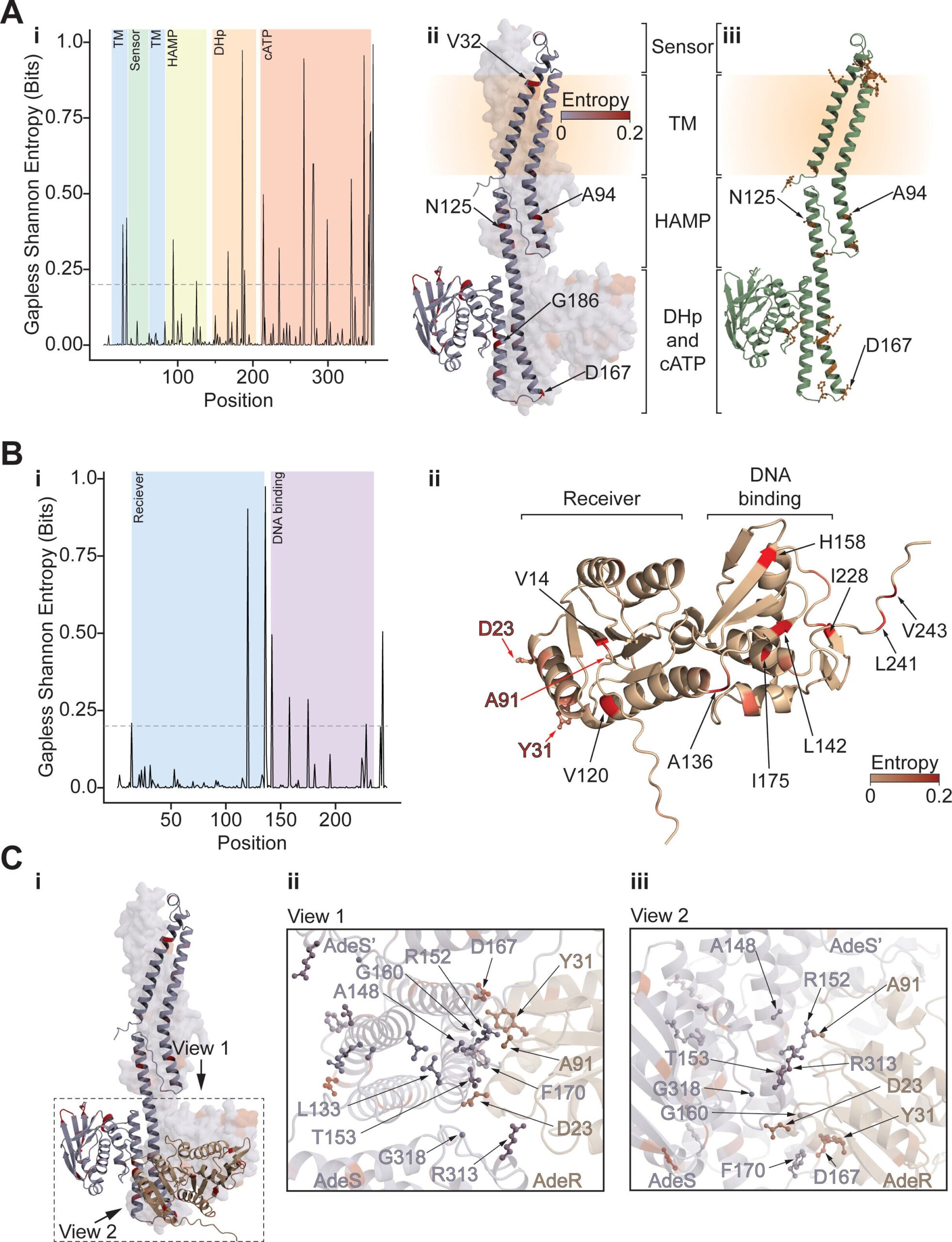
Regarding colistin resistance, the team identified mutations affecting the activity of a specific enzyme. These mutations hinder the enzyme’s ability to deliver the antibiotic to its intended target within the bacterial cell wall.
Predictive Genomics: A Path Towards Targeted Treatment
The researchers are optimistic that this newly acquired knowledge can be used to predict antibiotic resistance in clinical settings. By comparing their comprehensive map of resistance mutations with the genomes of bacteria isolated from patients, they can make predictions about drug susceptibility and inform treatment decisions.
“We now have access to over 10,000 publicly available genomes of A. baumannii isolates, which we have incorporated into our comparative analysis,” Osterman explained.
This research, combined with previous studies on antibiotic resistance in other pathogens, represents a significant step towards genomics-based predictions of drug resistance.
The Consequences of Trial-and-Error Treatment
The current practice of treating infections through trial and error – prescribing antibiotics without knowing whether the bacteria are already resistant – can inadvertently accelerate the spread of resistance. “When patients are treated with antibiotics to which the bacteria are already resistant, it further promotes resistance, and it wastes valuable time that patients may not have,” Osterman concluded. The ability to predict resistance profiles could revolutionize how clinicians approach treatment, paving the way for more targeted and effective therapies.